Background:
In Asia, treatment decisions in myelodysplastic neoplasms (MDS) are conventionally based on the Revised International Prognostic Scoring system (IPSS-R). A unique clinical-molecular prognostic model, the IPSS-molecular (IPSS-M), has been developed based on 2957 patients with de-novo MDS, therapy-related MDS, and MDS/myeloproliferative neoplasm (MPN) overlap syndrome. The IPSS-M comprises haematological parameters, karyotypic abnormalities and somatic mutations in a 31-gene panel. Validation of the IPSS-M in large multicentre studies in Asian has however not been performed. Hence, prognostic models taking into account the unique clinical-molecular characteristics of Asian MDS patients remain undefined.
Aims:
The objectives of this multicenter cohort study were: 1. to define the haematological, cytogenetic and molecular characteristics of Asian MDS patients; and 2. to develop a prognostic model based on these characteristics.
Methods:
Consecutive MDS patients in Hong Kong, Singapore and Taiwan diagnosed between 2004 to 2021 were studied. Data were censored on 17 September 2022. Patients with MDS/MPN overlap syndrome were excluded. A panel of 54 myeloid-related genes was sequenced in the diagnostic bone marrow by next-generation sequencing. Hematological, pathological, cytogenetic and molecular variables were evaluated for their association with overall survival (OS), leukemia-free survival (LFS), and time to progression to secondary acute myeloid leukemia (TTP-sAML). Variable selection was performed to determine the confounding variable and independent prognostic variables. The relative weights of the selected variables were estimated using a Cox multivariable model adjusted for confounders. According to the weights of each prognostic variable, individual patient-specific prognostic scores were calculated. Based on the scores of the entire cohort, six prognostic subgroups were defined. The statistical predictive power of this prognostic model was assessed by the concordance index (C-index). The prognostic model was validated with publicly available data from the IPSS-M cohort.
Results:
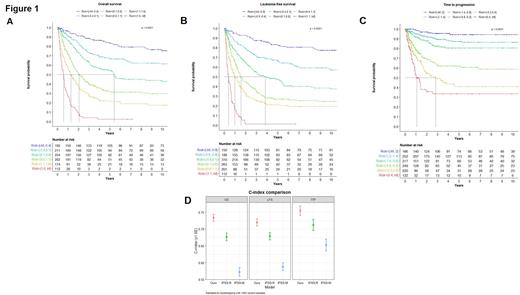
Seven hundred and seventy-eight men (63.5%) and 447 women (36.5%) at a median age of 68.4 (interquartile range, IQR: 57-77) years were studied. After a median follow-up of 2.85 (IQR: 0.97-7.06) years, there were 693 deaths (56.6%) and 284 transformations to sAML (23.2%). Three-hundred and ninety-four patients (32.2%) received hypomethylating agents (azaciticine, N=367; decitabine, N=27), and 158 patients (12.9%) underwent allogeneic haematopoietic stem cell transplantation. All patients showed at least one genetic alteration in the 54-gene panel (Figure 1A). Prognostic scoring systems (each with 6 prognostic subgroups) were established for OS (C-index: 0.72) (Figure 1A), LFS (C-index:0.71) (Figure 1B) and TTP-sAML (C-index: 0.74) (Figure 1C). Genomic factors significantly associated with inferior outcomes were monosomy 7, del(5q), and mutations in GNAS and TP53 for OS; trisomy 19, del(5q), monosomy 7, and mutations in GNAS, PTPN11 and TP53 for LFS, and i(17q), del(5q), and mutations in NPM1, NRAS, GNAS, IDH2, SF3B1, and RUNX1 for TTP-sAML. Using the IPSS-M publically available dataset as the validation cohort, our prognostic model gave C-indices of 0.70, 0.71 and 0.74 for OS, LFS and TTP-sAML respectively. Finally, this prognostic model had superior prognostic power as compared with the IPSS-R and IPSS-M for the current Asian cohort (Figure 1D).
Conclusion:
Combining genomic with hematological and cytogenetic parameters, the Asian clinical-molecular prognostic model improved the risk stratification of patients with MDS in Asia, potentially improving clinical decision-making.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal